PROTOCOL FOR SEPARATION OF PLASMA AND PERIPHERAL MONONUCLEAR CELL FRACTION FROM WHOLE BLOOD
For these blood draws we prefer the BD Vacutainer CPT tube, Becton Dickinson catalog # 362761- BD Vacutainer CPT Cell Preparation Tube with Sodium Citrate (available from Fisher Scientific, catalog #02-685-125). Carefully follow the instructions on the package insert for tube storage conditions and blood collection procedures.
At Study Site:
- Collect 8ml of blood via venipuncture directly into a BD Vacutainer CPT tube
- Invert the tube 10 times immediately after the draw (no shaking)
- Keep the tube upright and at room temperature
- Send tube to Johns Hopkins within 2 hours of blood draw. Alternatively, the tube can be spun at the study site and delivered to Johns Hopkins within 24 hours. The centrifuge used must achieve the recommended 1500-1800xg spin. If the tubes are spun at the study site, the tube should be inverted 5-10 times before transport to Johns Hopkins.
- See note below concerning the organization of case and control samples.
Hopkins Address:
Robert H. Yolken, MD
Johns Hopkins University – Stanley Division
600 N. Wolfe Street, Blalock 1105
Baltimore, MD 21287
410-614-0004
SHIPMENT OF SAMPLES
- For antibody testing, we prefer either serum or plasma.
- 0.5 mL minimum volume/sample, undiluted, is preferred. We can work with smaller volumes when necessary but this might result in fewer tests being performed.
- Samples should be frozen before and remain frozen during shipment (pack accordingly).
- We can also measure antibodies in whole blood samples that have been dried onto filter papers such as those commonly used for the measurement of metabolites in neonates.
- Filter paper samples must be atleast 5 millimeters in diameter.
- Samples (serum, plasma, or filter papers) can be sent in either 96-well U-bottom plates (preferable) or in tubes (serum or plasma only; do not send filter papers in tubes):
- Using microtiter plates generally results in a shorter turnaround time for receiving results.
- We recommend using a deep well plate similar to the 1.1 mL working volume plate made by Axygen (Mfr. # P-DW-11-D-S; VWR # 47734-788), shown below.
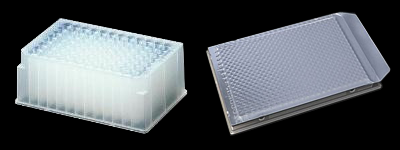
- Cover and seal the plates with an adhesive aluminum foil cover such as shown on the right above. (Example: USA Scientific # 2938-4100, Aluminum single tab sealing foil.)
- We recommend using a deep well plate similar to the 1.1 mL working volume plate made by Axygen (Mfr. # P-DW-11-D-S; VWR # 47734-788), shown below.
- We understand that sometimes samples must be sent in tubes. Please understand that this format is more labor intensive for our handling and will result in longer turnaround times for receiving results.
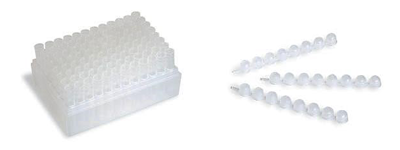
- If possible, we recommend using micro test tubes arranged in 96 well racks (example: BioRad Titertube #2239395) with plugs (BioRad #2239392)
- Make sure that each tube is clearly & securely labeled with the sample number that matches the sample list.
- We will accept samples in other types of tubes as well.
- Tubes with external screw caps are preferable
- If possible, we recommend using micro test tubes arranged in 96 well racks (example: BioRad Titertube #2239395) with plugs (BioRad #2239392)
NB: Proper labeling of plates and tubes is crucial and should exactly match the electronic version of the sample list emailed to us at the time of shipment! Plates should be clearly labeled numerically or alphabetically and preferably include the Study Title or Investigator’s last name. Tubes whose labels detach or are difficult to read are a common cause of unidentifiable samples. We will not test any samples from a set until all samples have been identified.
- Using microtiter plates generally results in a shorter turnaround time for receiving results.
- Sample orientation in 96 well [12 vertical columns (1 – 12) x 8 horizontal rows (A – H) plates or racks of tubes:
- Leave entire Column 1 EMPTY.
- Samples are arranged in vertical order, left to right beginning with position A2 (Row A, Column 2)) followed by B2, C2 and so forth.
- Sender may insert blanks or empty wells or tubes as desired but these should be noted as such in the sample list. SEE EXAMPLE BELOW for sample numbers 1 through 88.
Column Number Row 1 2 3 4 5 6 7 8 9 10 11 12 A Blank 1 9 17 25 33 41 49 57 65 73 81 B Blank 2 10 18 26 34 42 50 58 66 74 82 C Blank 3 11 19 27 35 43 51 59 67 75 83 D Blank 4 12 20 28 36 44 52 60 68 76 84 E Blank 5 13 21 29 37 45 53 61 69 77 85 F Blank 6 14 22 30 38 46 54 62 70 78 86 G Blank 7 15 23 31 39 47 55 63 71 79 87 H Blank 8 16 24 32 40 48 56 64 72 80 88
-
Sample list
- Send electronic version before the samples are shipped.
- Samples must be de-identified of personal information! The list, preferably on an Excel spreadsheet, should contain the list of sample numbers, sample volumes, sample location (plate map position, ex: plate 1, row A, column 2), and any other relevant information. Do not include name, social security number (or comparable), birthdates, or any other identifying information.
- Include a hardcopy of the list in the box with the samples.
- Send electronic version before the samples are shipped.
-
Shipment
Please contact us before shipping any samples to ensure that someone will be present to receive the samples and to track them down if there is a problem.
Please ship the samples to the following address:
Robert H. Yolken, MD
Johns Hopkins University-Stanley Division
600 N. Wolfe Street
Blalock 1105 (NOTE: THIS IS THE MOST IMPORTANT PART OF THE ADDRESS)
Baltimore, MD 21287
410-614-0004Samples should be shipped on dry ice, with enough dry ice for at least 3 days in shipping and storage. Federal Express is the preferred shipper.
It is recommended that you ship samples on Monday or Tuesday to avoid problems associated with the location of samples over the weekend.
ORGANIZATION OF SAMPLES WITHIN PLATES / RACKS
Samples are run on microplates in sets of up to 88 samples. We make every effort to standardize the conditions of the runs across sets. However, it is difficult, if not impossible, to totally eliminate such differences, which are similar to “platform” effects seen in most solid phase assays. It is particularly difficult to eliminate the platform effects in large-scale studies where large numbers of samples are run over an extended period of time. In such cases, it is crucial that there be no bias in terms of samples run early in the study versus those run late in the study. The best way to avoid the effects of such bias is to have the samples assigned to the plates in random order. An alternative in case-control studies is to assign the same number of cases and controls to each plate. This allows for the use of a number of normalization routines as well as statistical methods, such as conditional logistic regression, which allows for comparisons within each plate or run. What needs to be avoided are sample sets in which all of the cases are run on one set of plates and all of the controls on another, making meaningful standardization across plates difficult, if not impossible.
SAMPLE TESTING
We generally run assays in panels. The composition of the panels could vary depending upon availability of assay reagents and the interests of the investigators. All assays are for IgG class antibodies unless otherwise specified.
- Primary Panel
- Herpes simplex virus Type 1 (HSV-1)
- Herpes simplex virus Type 2 (HSV-2)
- Cytomegalovirus (CMV)
- Toxoplasma gondii IgG
- C-Reactive Protein (CRP)
- Secondary Panel
- Epstein Barr Virus (EBV-EBNA)
- Varicella Zoster Virus (VZV)
- Toxoplasma gondii IgM
- Human herpesvirus 6 (HHV-6)
- Influenza A virus (H3N2)
- Influenza B virus
- Gliadin IgG
Additional assays may be performed based on the interest of the investigators.
Results are reported electronically on a sheet which contains our laboratory ID number as well as the ID number provided by the investigator. The results are generally presented as quantitative values which are derived from the level of reactivity and standards run with each assay, as well as qualitative results listed as “positive”, “negative”, or “equivocal”. We also generally provide an overall estimation of the prevalence of antibodies in your population and comparison with other populations that we have tested.
